Pathophysiology of Shock
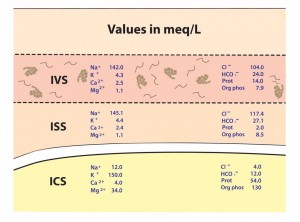
In a normal human physiologic state, there is a homeostasis that exists in cells that includes good stores of energy (e.g. ATP) and energy sources (e.g. glucose), an adequate supply of oxygen, and a pH , fluid, and electrolyte balance that optimizes cellular function. About 20% of the energy expended in the body at rest, that is 20% of the basal metabolic rate (BMR), is used to maintain Na+ and K+ gradients via the Na+/K+ ATPase pump. In fact, the brain and kidneys use 50 – 70% of their BMR on this function. If any of the conditions above are disrupted, say by lack of blood flow to cells of the body, cellular dysfunction occurs. If disruption persists for a long enough period of time functions, such as the Na+/K+ ATPase pump on the cell membrane, begin to fail and Na+ and K+ (along with fluid) follow diffusion gradients and begin to equilibrate between the intracellular space and interstitial space. Homeostasis is lost, enzymes fail to function properly, and cellular death occurs. The goal, then, is to recognize and treat shock when it first manifests. This will decrease morbidity and mortality in your patients.
So, what is shock? Clearly stated, shock is defined as a decrease in circulation of oxygen and/or nutrients to tissues to the point that those tissues malfunction, become damaged, and ultimately, in severe cases, are destroyed. In order to avoid shock, then, one must have adequate blood flow to the tissues, and that blood has to be carrying adequate oxygen and nutrients. In resuscitation of any critically ill or injured patient, the physician must address the ABC’s: i.e. Airway, Breathing, and Circulation. If the patient cannot maintain a clear airway, one must be provided, often by placement of an endotracheal tube. Breathing, if inadequate, must be assisted. If the patient is hypoxic (has low oxygen in the blood), supplemental oxygen is administered as well. The third component of this triad, circulation, is central to the pathophysiology and treatment of shock.
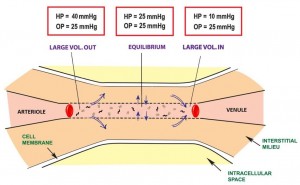
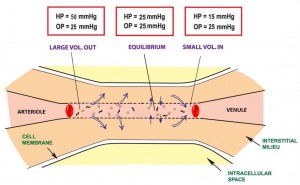
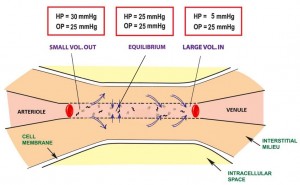
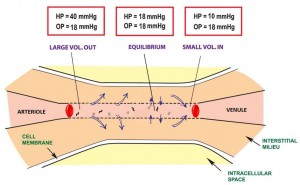
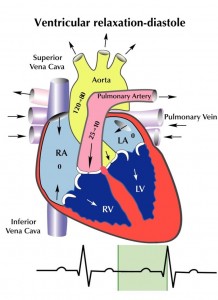
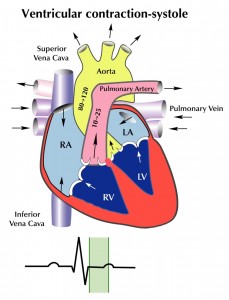
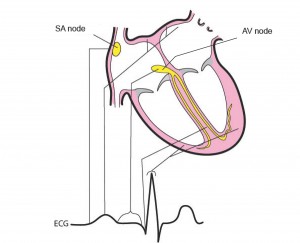
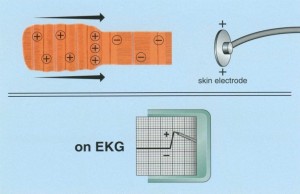
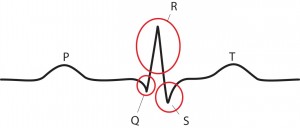
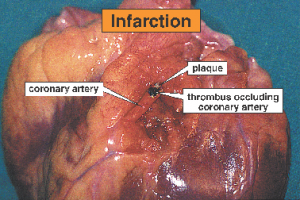
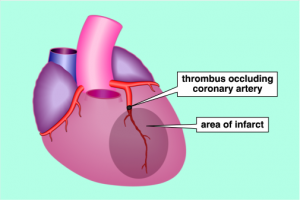
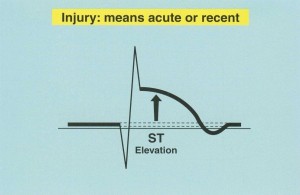
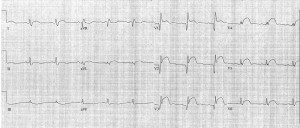
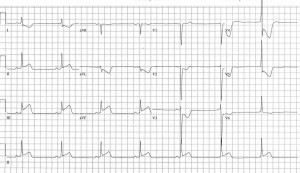
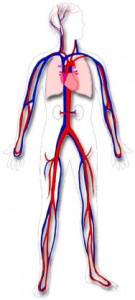
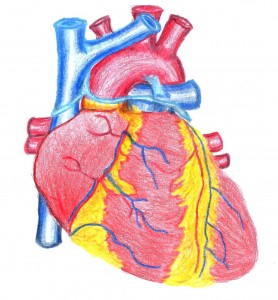
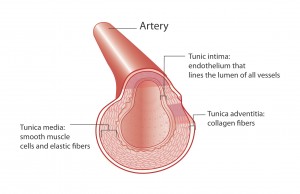
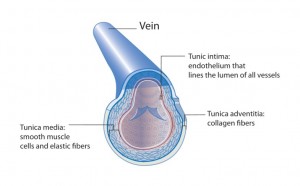
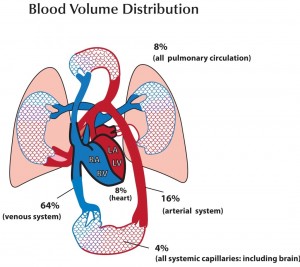
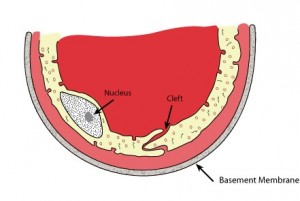
There are three factors that determine blood flow to tissues: blood volume, “pump function” (cardiac function), and vascular capacitance and resistance. Low blood volume, due to hemorrhage or dehydration, results in a decrease cardiac output because there is a decrease in stroke volume. When hydrostatic pressure is reduced to the point that perfusion to the body is compromised, we call this hypovolemic shock. Cardiogenic shock is poor tissue perfusion as a result of the heart not functioning well. This decrease in cardiac output can be the result of decreased stroke volume (e.g. from a heart attack and impaired contractility of the heart muscle), a low heart rate (e.g. from an unfavorable drug effect), or valve dysfunction, where forward flow of blood is impeded. Vasogenic shock refers to decreased perfusion to the core of the body because of some problem with vascular tone. Under normal circumstances there is vascular tone, or slight vasoconstriction, to the extremities. This is because they do not need a lot of blood flow when at rest. When we exercise, additional flow is needed in the extremities and thus we increase our cardiac output, by increasing our heart rate, to accommodate this need. There are conditions, though, that occur when there is abnormal dilatation of the blood vessels (e.g. toxic effect of drugs), where perfusion to the core is compromised because of dilatation of arteries to the periphery. In the case of bad infections, sepsis, there can also be leakage of fluid from capillaries because of effects of certain conditions created. In this instance, intravascular proteins can be leaked into the interstitial space and fluid will be drawn out of the vascular space (since there is a loss of intravascular oncotic pressure). These vascular problems result in vasogenic shock.
There is one more type of shock that does not fit neatly into any of the above categories and that is something commonly referred to as mechanical shock. In this instance, there is impedance of blood flow as a result of something physically impairing blood flow. This can be the result of a collapse of the lung causing a tension pneumothorax, pulmonary emboli, cardiac tamponade, or some kind of mass or tumor compressing a major vessel from the outside and impairing flow. Again, when any of these conditions exist, we refer to this kind of shock as, mechanical shock.
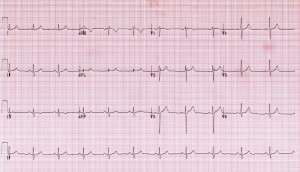
The human body has some ability to compensate for adverse conditions leading to shock, e.g. heart rate can increase to improve cardiac output, blood vessels to the extremities can constrict to shunt blood preferentially to important organs (heart, lungs, and brain), and the nervous system can give a sense of thirst and distress. Compensatory mechanisms, however, can quickly become overwhelmed, and a state of non-compensatory shock sets in. If conditions do not improve promptly, terminal shock ensues, organs fail, and the victim dies. These are the 3 stages of shock: 1. Compensatory, 2. Non-compensatory, and 3. Terminal. Compensatory shock can be subtle. The patient may be mildly anxious, diaphoretic (sweaty), and tachycardic (defined as a heart rate greater than 100 beats per minute in a normal adult). The blood pressure will be normal or near normal (systolic pressure about 110 to 130 mmHg for normal adult) and the patient will be mentating normally. During compensatory shock, the body is releasing endogenous catecholamines (e.g. epinephrine from the adrenal glands) in an effort to increase cardiac output and constrict blood vessels leading to the skin and extremities and shunt blood preferentially to the abdomen, chest, and brain. In addition, the kidneys are attempting to retain as much fluid as possible, so urine output decreases. As conditions worsen, compensatory mechanisms begin to fail. Catecholamine stores are depleted, renal function fails because of poor perfusion, and the patient’s blood pressure drops further. If the cause of shock is not targeted soon and treated, the patient will progress to terminal shock and ultimately die. Terminal shock is a condition in which cellular function is actively failing because of poor perfusion to the tissues.
The treatment of shock is straightforward: identify that the patient is in shock, find the cause of shock, and treat the underlying condition of causing shock. After stabilization of the patient’s condition, provide supportive care to sustain a more normal physiologic state. With this fund of new knowledge, let’s take a look at our original case scenario that started this chapter and see if we can save his life!